It is a fact of life in the world of New York State Workers’ Compensation that getting medication is not as easy as your everyday trip to the pharmacy to pick up a prescription. One of the main reasons for this is the number of parties involved, and the regulatory structure under which those parties do business.
We tend to think of the medications which we take as a private business between our doctors and ourselves. Although we are aware that our private health insurance has a say in what will and will not be paid for, the Doctor is well aware of those particular restrictions, and will prescribe accordingly, keeping the prescription machine flowing smoothly enough that being able to obtain a prescription is relatively easy.
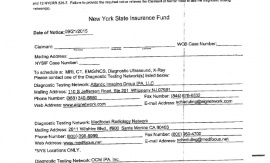
For compensation claimants, there are not only more parties that stand between you and your medication, there is the additional regulatory filter of the New York State Medical Treatment Guidelines. These are guidelines that all parties involved must adhere to.
For the Workers’ Compensation claimant it may be better to think of a prescription as a request, rather than Doctor’s Orders. It is a request that has to pass through all parties involved in order to be granted.
Here is an overview of the general process:
John M. Bellinger
Paralegal
Email: jbellinger@mcvlaw.com
This entry was written by John Bellinger, who is part of the Worker’s Compensation team at MCV Law.
 MCV Law Email Sign Up
MCV Law Email Sign Up




What should I do if I have been in a motor vehicle accident...











Guillain Barre Syndrome (“GBS”) is a very serious autoimmune...